Nutrition plays a crucial role in maintaining health, well-being, and independence for elderly individuals. Unfortunately, many older adults face a range of nutrition-related issues that can lead to serious health consequences if left unaddressed. For aged care providers, families, and allied health professionals, understanding the common dietary challenges in the elderly and applying effective interventions is essential.
This article explores these frequent issues and shares proven strategies to improve nutrition in the elderly, ensuring quality care and better outcomes.
Common Dietary Challenges in the Elderly
As people age, physiological and social changes often impact their ability to maintain adequate nutrition. Among the most prevalent problems are malnutrition in aged care and dysphagia.

Malnutrition affects a significant number of elderly people, especially those living in residential aged care or managing multiple chronic conditions. It can result from decreased appetite, difficulty chewing or swallowing, or side effects of medication. Malnutrition not only weakens the immune system but also increases the risk of falls, delays wound healing, and can reduce overall quality of life.
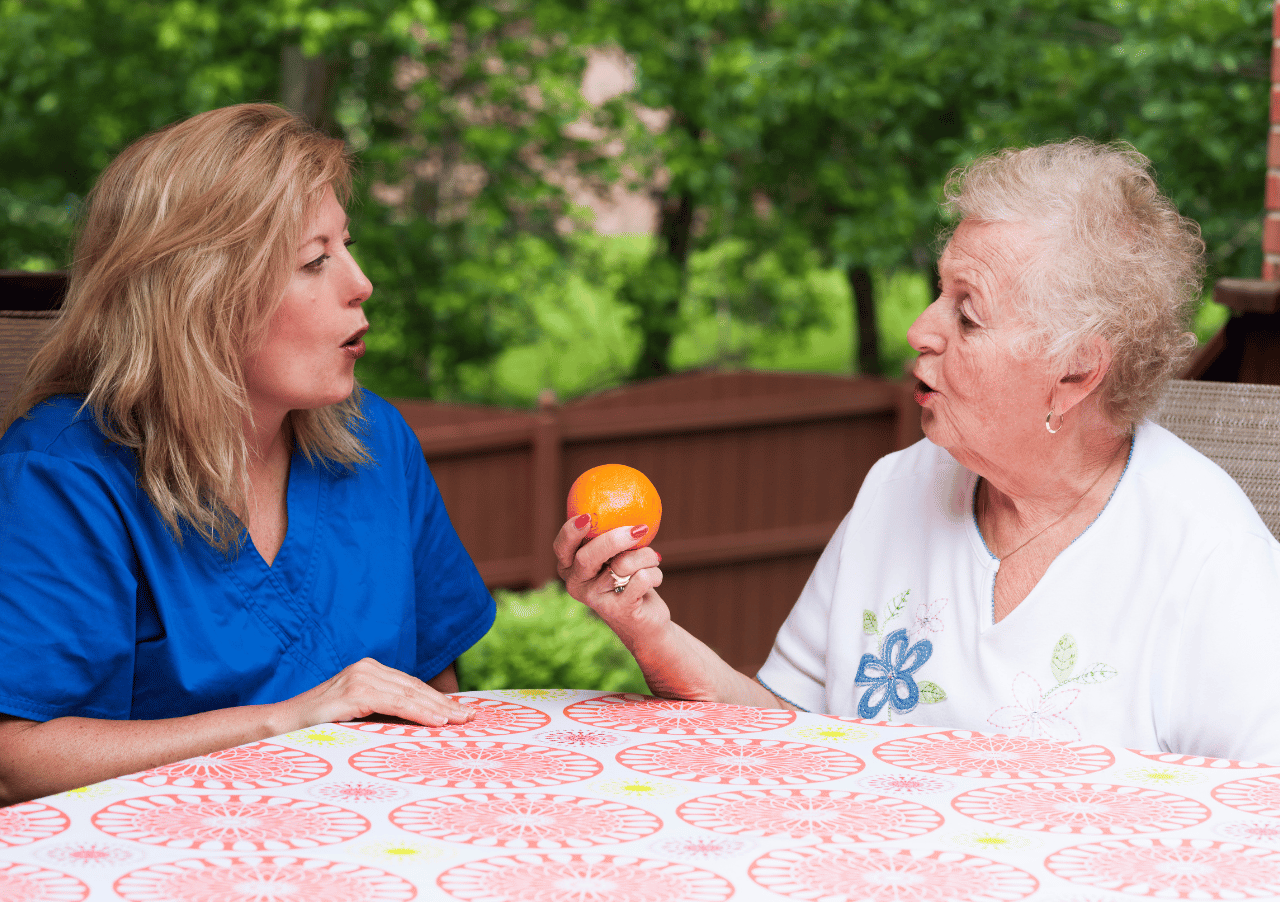
Dysphagia, or difficulty swallowing, is another critical concern. It affects many elderly people due to neurological conditions, stroke, or natural muscle decline. Dysphagia increases the risk of choking and aspiration pneumonia, and often leads to inadequate food and fluid intake.
Other common dietary challenges in the elderly include sensory changes such as reduced taste and smell, dental problems limiting food choices, and social isolation which can decrease motivation to eat. Medications may also interfere with appetite or nutrient absorption, complicating nutritional status further.
Why Addressing Nutrition in Aged Care Requires a Multidisciplinary Approach
Nutrition challenges in aged care are rarely straightforward and often require a team effort to manage effectively. This is where the value of a multidisciplinary approach comes into play, involving physiotherapists, dietitians, occupational therapists, nurses, and other allied health professionals.
For example, physiotherapists can support mobility and muscle strength, enabling elderly individuals to feed themselves independently. Dietitians provide tailored meal planning and nutritional assessments to address deficiencies or special dietary needs. Occupational therapists help with adaptive tools or strategies for safe eating and drinking, especially for those with dysphagia.
At AHP Aged Care, we embrace this comprehensive model, working collaboratively with aged care providers to deliver personalised, scalable solutions. This integrated care ensures that strategies to improve nutrition in the elderly address physical, medical, and social factors holistically.
Strategies to Improve Nutrition in the Elderly
Implementing effective strategies to improve nutrition in the elderly requires a combination of assessment, intervention, and ongoing monitoring.
- Regular Nutritional Screening and Assessment
Early identification of nutritional risks through validated screening tools is vital. These assessments should include weight monitoring, dietary intake analysis, and checks for swallowing difficulties. The Australian Government Department of Health emphasises the importance of nutritional care in aged care facilities, recommending routine screening to prevent malnutrition and associated complications. - Personalised Meal Planning
Tailoring meals to individual preferences, cultural considerations, and dietary restrictions helps improve food intake and satisfaction. Providing a variety of textures and flavours can stimulate appetite, especially for those experiencing sensory changes. - Dysphagia Management
For those with swallowing difficulties, modified texture diets and specialised swallowing therapy are critical. Occupational therapists play a key role in assessing swallowing function and training both clients and care staff in safe eating techniques. - Encouraging Hydration and Balanced Nutrient Intake
Dehydration is common among elderly populations and often overlooked. Promoting regular fluid intake alongside meals, offering nutrient-dense snacks, and supplementing when needed are all practical interventions. - Enhancing the Dining Environment
Creating a pleasant, social atmosphere during mealtimes can encourage eating. Simple changes like communal dining, minimising distractions, and ensuring comfortable seating can boost appetite and food consumption. - Staff Training and Education
Care staff must be equipped with knowledge about nutrition issues, signs of malnutrition, and effective feeding techniques. Ongoing education ensures early identification of problems and timely interventions.
Practical Interventions to Implement in Aged Care Settings
Putting these strategies into practice involves close collaboration between aged care providers and allied health specialists.
- Collaborative Care Planning
Working together to develop and review individual nutrition care plans ensures they remain relevant and effective. - Use of Nutritional Supplements and Specialised Products
For residents unable to meet their nutritional needs through food alone, supplements and specialised products can bridge gaps, but they must be carefully selected and monitored. - Ongoing Monitoring and Adjustments
Nutrition is dynamic, especially in aged care where health status can change rapidly. Regular reviews allow timely changes to dietary plans or therapy.
How AHP Aged Care Supports Aged Care Providers with Nutrition and Allied Health Services
At AHP Aged Care, we understand the complexities surrounding elderly nutrition and offer tailored, multidisciplinary solutions designed to improve health outcomes. Our experienced team of dietitians, physiotherapists, occupational therapists, and other allied health professionals collaborate closely with aged care providers to deliver strategies to improve nutrition in the elderly that are practical, scalable, and personalised.
We provide workforce solutions that allow facilities to implement specialised therapy and nutrition interventions effectively, ensuring clients receive the support they need to maintain independence and quality of life.

Addressing common dietary challenges in the elderly is essential to prevent malnutrition, support health, and enhance quality of life in aged care settings. By applying evidence-based strategies to improve nutrition in the elderly, care providers can meet the complex needs of their residents through comprehensive, personalised interventions.
AHP Aged Care’s multidisciplinary approach ensures these challenges are managed holistically, combining expertise across allied health fields to deliver practical, impactful nutrition care. Through ongoing assessment, tailored meal planning, dysphagia management, and collaborative care, aged care facilities can create a supportive environment that promotes better nutrition and well-being.